The standard of active humidification in non-invasive ventilation redefined
In acute exacerbations of chronic obstructive pulmonary disease (COPD), non-invasive ventilation (NIV) is one of the preferred treatment methods. Often, the tolerability and success of NIV are directly related to the patient’s well-being – an essential accompanying factor for the success of therapy. It is undisputed that humidification has long been a standard part of invasive mechanical ventilation, because the constant administration of cool and dry ventilation gas can lead to serious complications such as mucociliary dysfunction and, under certain circumstances, blockage of the endotracheal tube.

Humidification is strongly recommended for both invasive and non-invasive ventilation
NIV is used in a wide range of treatments: from continuous positive pressure ventilation (e.g., as part of sleep apnea therapy at home) to intensive respiratory support in the hospital.
The success of NIV in combination with active humidification is reflected in the improvement of the patient’s well-being by making breathing easier. Without active humidification, patients complain more frequently of dry mouth – usually caused by the continuous cooling and associated drying of the airways during therapy. As a result, airway resistance increases. Breathing becomes more difficult.

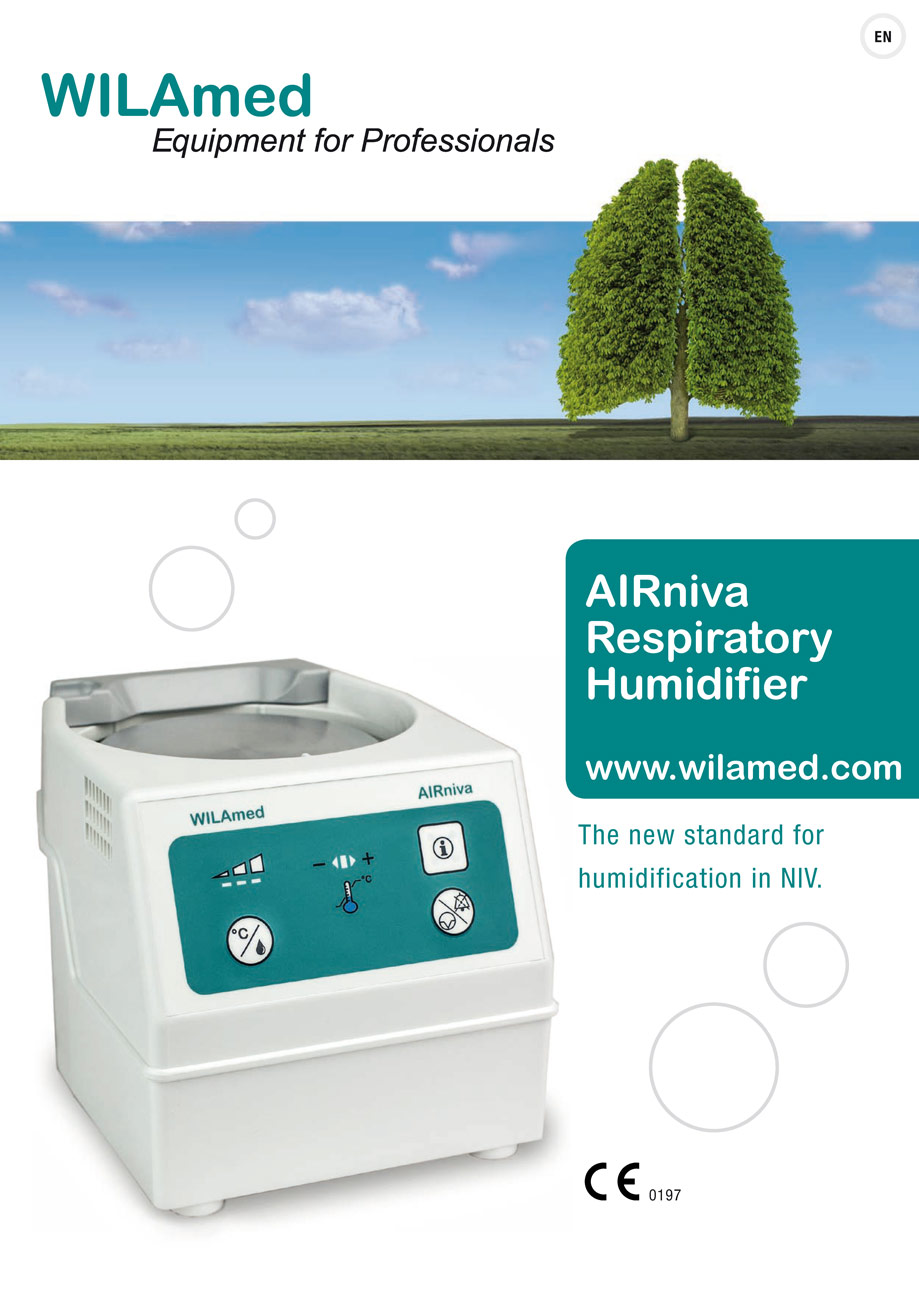
The new AIRniva respiratory gas humidifier from WILAmed supplies machine-ventilated patients with conditioned respiratory gas in a simple and safe manner and helps to improve patient tolerance of NIV treatment.
Product information