How does natural breath conditioning work?
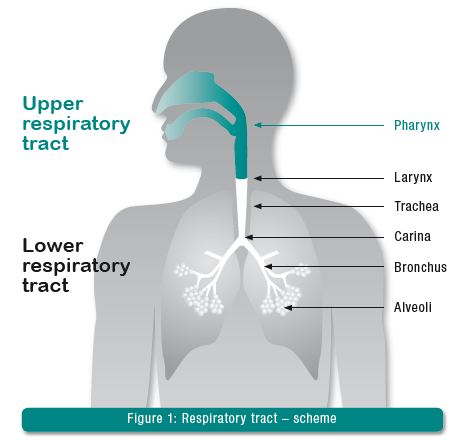
In healthy individuals, 75% of respiratory gas conditioning takes place in the upper respiratory tract (nasopharynx). The remaining 25% is provided by the trachea. Every day, the upper respiratory tract heats, humidifies and cleans 1,000-21,000 liters of respiratory gas, depending on body size and physical capacity.
1. Warming
The breathing air is heated by many small blood vessels that cover the nasal and oral mucosa like a network. Nerve impulses regulate the amount of blood flowing through them like the body’s own heating system. Thus, the vessels are supplied with more blood when the air is cold (warming the respiratory gas) and less when the air is warm.
2. Humidification
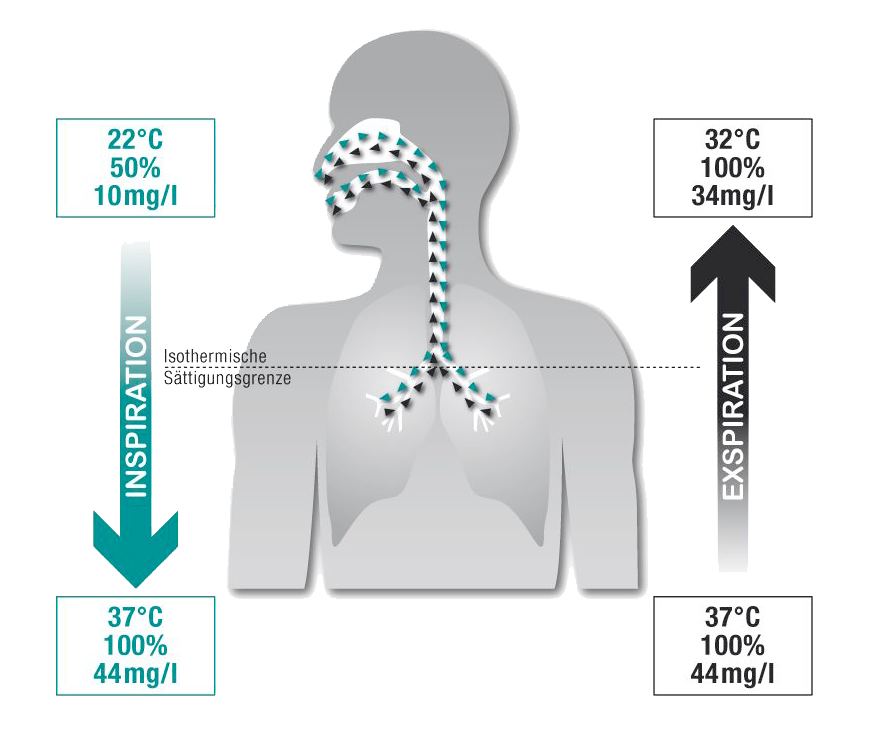
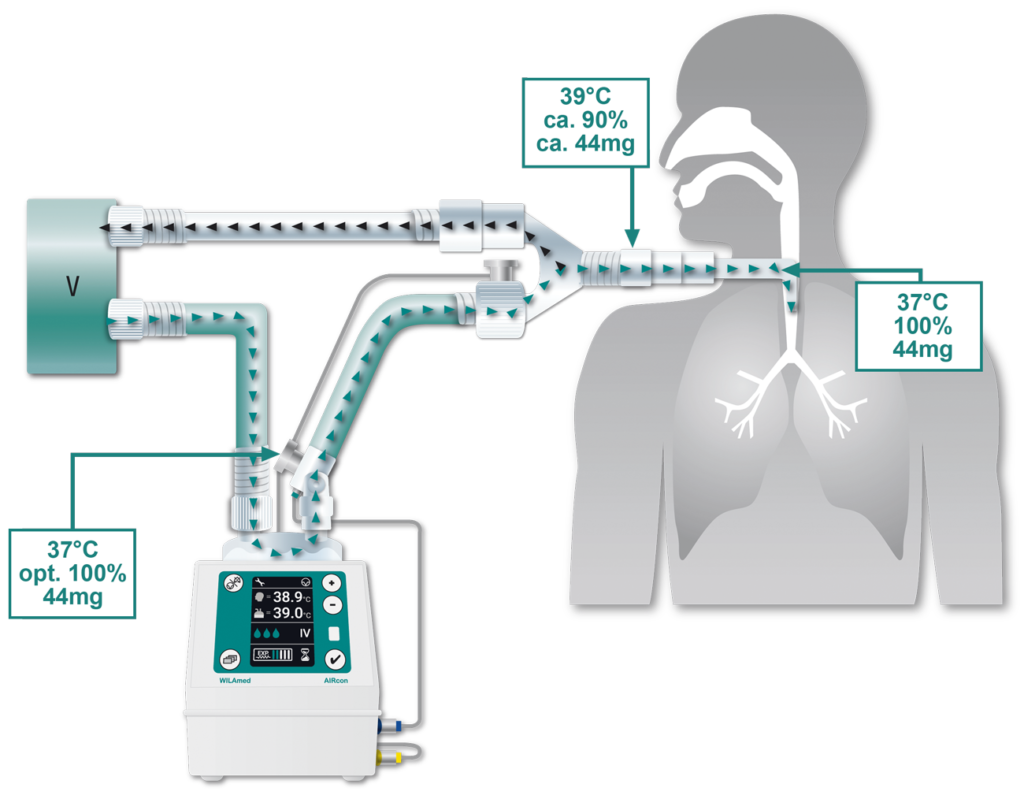
During inspiration, the mucous membrane inside the nose and in the mouth, which is well supplied with blood, releases moisture into the passing respiratory gas. As a result, 200 to 300 ml of water evaporate daily in healthy adults. During inspiration through the nose or mouth, the mucous membranes cool down. This cooling causes some of the moisture in the air coming out of the lungs (100% humidity at 37°C) to condense on the mucous membranes during exhalation. The mucous membranes are thereby re-moistened. On its way into the lower respiratory tract, the respiratory gas already humidified in the nasopharynx is further conditioned until the isothermal saturation limit is reached. The isothermal saturation limit is the maximum possible humidity at a given heat. At 37°C body core heat, this corresponds to a relative humidity of 100% or 44 mg/l absolute humidity. In a healthy person breathing calmly, this equilibrium is reached when breathing through the nose at the bifurcation of the trachea. This ensures that only air saturated with water vapor and warm to the body reaches the alveoli.
3. Cleaning
While the removal of inhaled particles in the upper respiratory tract takes place primarily through coughing and sneezing (tussive clearance), the focus in the deeper respiratory tract is on mucociliary clearance. It is the most important cleansing mechanism of the bronchi.
Mucociliary Clearance
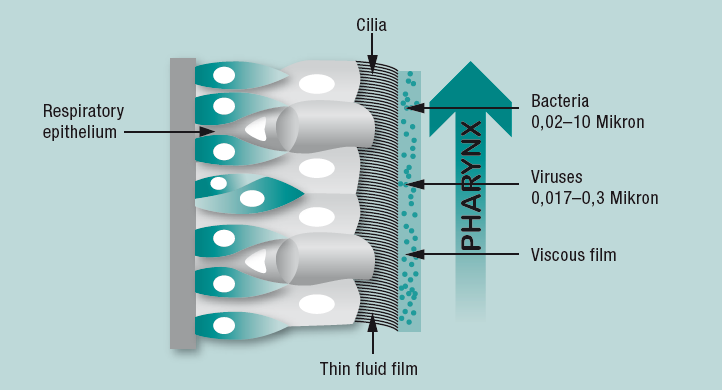
The main bronchi up to the alveoli are lined with a respiratory epithelium. On it are ciliated cells bearing hair-shaped structures (cilia) on their surface. The cilia are surrounded by a thin fluid layer of mucus. On top of this is a second viscous mucus layer in which foreign particles and microorganisms adhere.
The cilia perform movements within the thin-liquid mucus layer in a coordinated manner in the direction of the pharynx. This transports the viscous mucus layer toward the mouth, where it is swallowed or coughed up. Optimal function of mucociliary clearance requires a temperature of 37°C and an absolute humidity of 44 mg/l corresponding to a relative humidity of 100%. If there is insufficient heat and humidity in the lower airways, the ciliated cells cease their transport function after a short time. Bacterial colonization is facilitated under these conditions.
When is respiratory gas conditioning affected?
Mechanical ventilation, especially with dry, cold respiratory gases, restricts and partly bypasses natural respiratory gas conditioning. With non-invasive ventilation (e.g., breathing masks), a continuous positive flow is often administered (e.g., CPAP). The resulting increased mouth breathing may cause undesirable side effects. In the long term, the upper airways dry out due to the permanent supply of cool respiratory gases. The consequences are painfully inflamed nasal and oral mucous membranes as well as blockages of the airways and congestion of secretions in the respiratory system.
Leakage from the breathing mask in particular can promote drying of the nasal mucosa. A continuous supply of warm respiratory gases contributes to the substantial alleviation of this clinical picture. Invasive ventilation (intubation or tracheostomy) bypasses the upper airway and prevents it from performing its natural function. Respiratory gas conditioning is then shifted exclusively to the trachea, which, however, cannot provide the necessary humidification, warming and cleansing services on its own.
The challenges with mechanical ventilation are:
Insufficient heating capacity
Breathing gas that is not sufficiently heated enters the lungs.
Insufficient humidification performance
The insufficiently heated air cannot transport the required amount of moisture due to the isothermal saturation limit.
Restricted cleaning of the respiratory tract
Ventilation with excessively cold and dry respiratory gases causes the mucus on the respiratory epithelium to become more viscous within a very short time, which impairs the function of the ciliated cells. The beating frequency of the cilia slows down to eventual sistasis (at <30% water vapor saturation after 35 min). After one hour at the latest, damage is detectable in the cell smear.
This can have serious consequences:
- Impairment of ciliary function due to viscous mucus and swelling of mucous membranes
- Increase in airway resistance and decrease in compliance due to increasing secretion congestion as well as incrustations.
- Risk of atelectasis due to reduced surfactant activity
- Impediment of gas exchange in the lungs
- Increased susceptibility to pulmonary infections
Premature infants are particularly vulnerable to such complications. From the 24th week of pregnancy, they are already viable, but their lungs, bronchial tree and mucociliary clearance are still extremely underdeveloped. In addition, they must immediately adapt to a cooler and drier environment. Even after birth, ontogenetic development is not yet complete. To prevent dehydration or hardening of the lungs, optimal respiratory gas humidification is imperative in ventilated preterm infants and neonates.
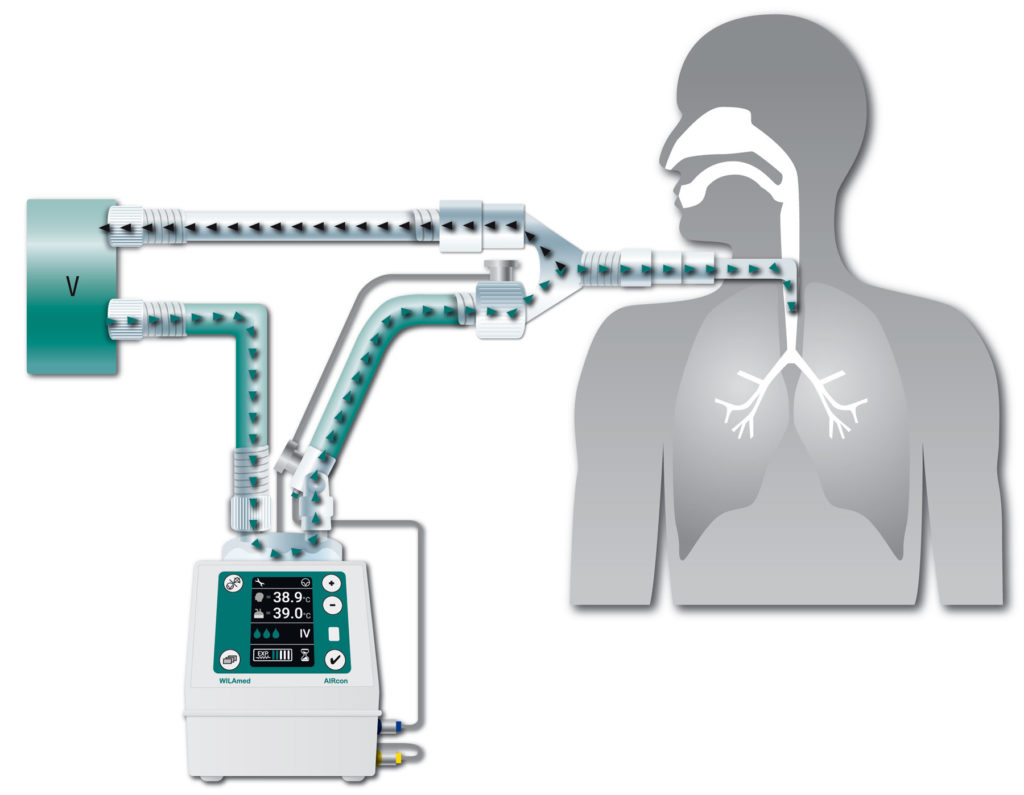
Operating principle of the AIRcon respiratory gas humidifier
If a patient is ventilated for an extended period of time, it is imperative that measures be taken to compensate for heat and moisture loss to avoid the complications listed above.
The AIRcon humidifier compensates for this heat and moisture loss. The dry and cold inspiratory air from the ventilator is fed into the humidifier chamber of the AIRcon. There it flows over the water surface and absorbs heat and moisture in the form of water vapor (pass over process). Since water vapor cannot transport germs, the risk of contamination is considerably reduced. The conditioned inspiratory air is then passed to the patient. A heating wire embedded in the breathing tube continues to keep the temperature constant and prevents condensation in the tube.
In this way, the AIRcon keeps the mucus layer of the respiratory epithelium supple and the cilia mobile. Foreign particles and microorganisms that may lead to pulmonary infections or lung tissue damage can be successfully removed.
Advantages of the AIRcon humidifier over HMEs
Humidifier chamber
Mountings
Breathing Tube Systems
References
1 W. Oczenski, H. Andel und A. Werba: Atmen Atemhilfen. Thieme, Stuttgart 2003: 274, ISBN 3131376961.
2 A. Wanner, M. Salathé, T.G. O‘riordan: Mucociliary Clearance in the Airways. In: American journal of respiratory and critical care medicine, 1996, 154 (1), no6: 18681902, ISSN 15354970.
3 N. Cauna, K.H. Hinderer: Fine structure of blood vessels of the human nasal respiratory mucosa. In: Ann Otol Rhinol Laryngol, 1969; 78(4):86579, ISSN 00034894.
4 J. Rathgeber, K. Züchner, H. Burchardi: Conditioning of Air in Mechanically Ventilated Patients. In: Vincent JL. Yearbook of Intensive Care and Emergency Medicine, 1996: 501519, ISSN 09425381.
5 M.P. Shelly, G.M. Lloyd, G.R. Park: A review of the mechanism and methods of humidification of inspired gases. In: Intens Care Med. 1988; 14:1, ISSN 03424642.
6 M.A. Sleigh, J.R. Blake, N. Liron: The Propulsion of Mucus by Cilia. In: Am. Rev. Respir., Dis. 1988; 137: 72641, ISSN 00030805.
7 R. Williams, N. Rankin, T. Smith, et al. Ralationship between humidity and temperature of inspired gas and the function of the airway mucosa. In: Crit. Care Med, 1996, Vol. 24, no11: 19201929, ISSN 00903493.
8 R. Estes, G. Meduri: The Pathogenesis of Ventilator Associated Pneumonia: 1. Mechnisms of Bacterial Transcolonization and Airway Innoculation. In: Intensive Care Medicine. 1995; 21: 365383, ISSN 03400964.
9 H. Schiffmann: Humidification of Respired Gases in Neonates and Infants. In: Respir Care Clin. 2006;12:321336, ISSN 10785337.
10 S. Schäfer, F. Kirsch, G. Scheuermann und R. Wagner: Fachpflege Beatmung. Elsevier, München 2005, S. 145146, ISBN 3437251821
11 M.T. Martins de Araújo, S.V. Vieira, E.C. Vasquez, et al. Heated Humidification or Face Mask To Prevent Upper Airway Dryness During Continuous Positive Airway Pressure Threapy. In: Chest. 2000; 117: 142147, ISSN 00123692.